营养支持
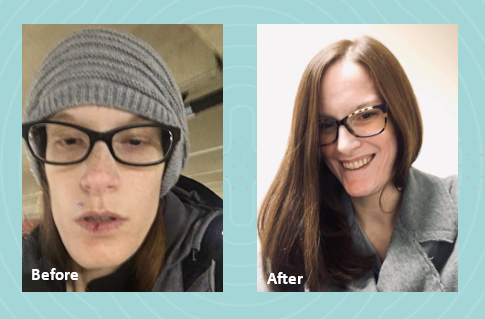
In 2022, I graduated from nursing school with dreams of starting my career as a nurse. However, life had other plans. I was diagnosed with gastroparesis, a condition that made it impossible for me to work and pursue my passion. As my condition worsened, I had to put my career on hold to focus on my health.
 Initially, my local clinicians recommended jejunal feedings, which I tolerated well at first. However, after my J-tube surgery, my condition began to deteriorate, and eventually I became severely malnourished. I was surviving on a mere 500 calories a day, leaving me too weak to perform even the simplest tasks. My mom had to help me with everything, including bathing. Living in a two-story home became a daily struggle, as I had to crawl up the stairs, feeling my body slowly giving up.
Initially, my local clinicians recommended jejunal feedings, which I tolerated well at first. However, after my J-tube surgery, my condition began to deteriorate, and eventually I became severely malnourished. I was surviving on a mere 500 calories a day, leaving me too weak to perform even the simplest tasks. My mom had to help me with everything, including bathing. Living in a two-story home became a daily struggle, as I had to crawl up the stairs, feeling my body slowly giving up.
My local registered dietitian recommended Parenteral Nutrition (PN) and sent the order. We were then referred to Option Care Health (OPCH). I was scared to start PN, but my OPCH dietitian reassured me, saying, “Just because you’re on PN doesn’t mean your life is over. The goal is to give you back more of your life than before.” Her words stuck with me, offering hope during a difficult time.
Due to my blood sugar issues, I’m on 23-hour PN feeds and carry a backpack that has become a part of me. Despite these challenges, my OPCH team has been incredible. My registered dietitian and pharmacist have truly been lifesavers. I continue to speak with my OPCH registered dietitian weekly because she genuinely cares about my well-being and supports me through every step of my journey.
Thanks to the unwavering support of my Option Care Health team and my local registered dietitian, I am back to work and feeling so much better. I wholeheartedly recommend Option Care Health to anyone in need. They have played a crucial role in my recovery, and I am forever grateful for their dedication and care.

营养支持
Gastroparesis refers to a delay in emptying stomach contents. Symptoms often include feeling full after eating a meal, or even a small amount of food, as well as nausea, vomiting, bloating or abdominal pain. The causes of gastroparesis may include diabetes mellitus, complications after surgery, kidney disease, certain medications, thyroid disorders, cancer, among others.
The following tips are intended to reduce symptoms and help maintain adequate nutrition.
|
Mealtime
|
||
|
Foods
|
|
|
Fluids
- Stay hydrated. Most adults need 6-10 cups of water per day. Sip slowly throughout the day.
- Drink fluids with meals, however; be sure not to fill up on liquids
- Avoid carbonated beverages as they can cause bloating
其他
- Avoid alcohol as it can affect stomach emptying
- Foods that are acidic, spicy, or contain caffeine or mint may increase acid reflux
- Keep blood sugars under control if you have diabetes
- Keep a food diary to track your intake and find foods that are best tolerated
- Exercise may increase stomach emptying and reduce symptoms. Walking after meals is suggested.
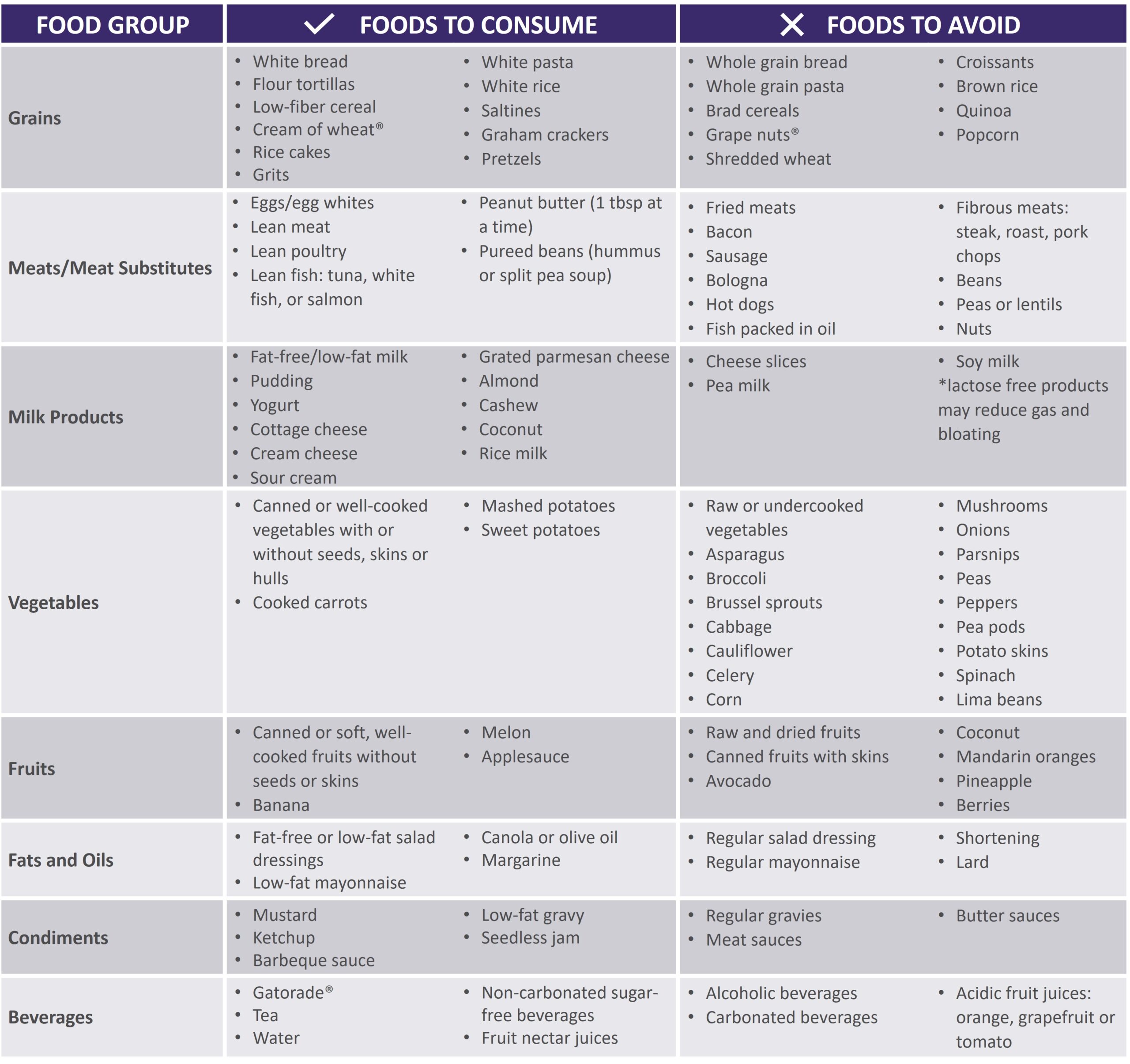
See below for help in choosing more optimal foods from each food group:
 |
|
Gastroparesis Sample Menus |
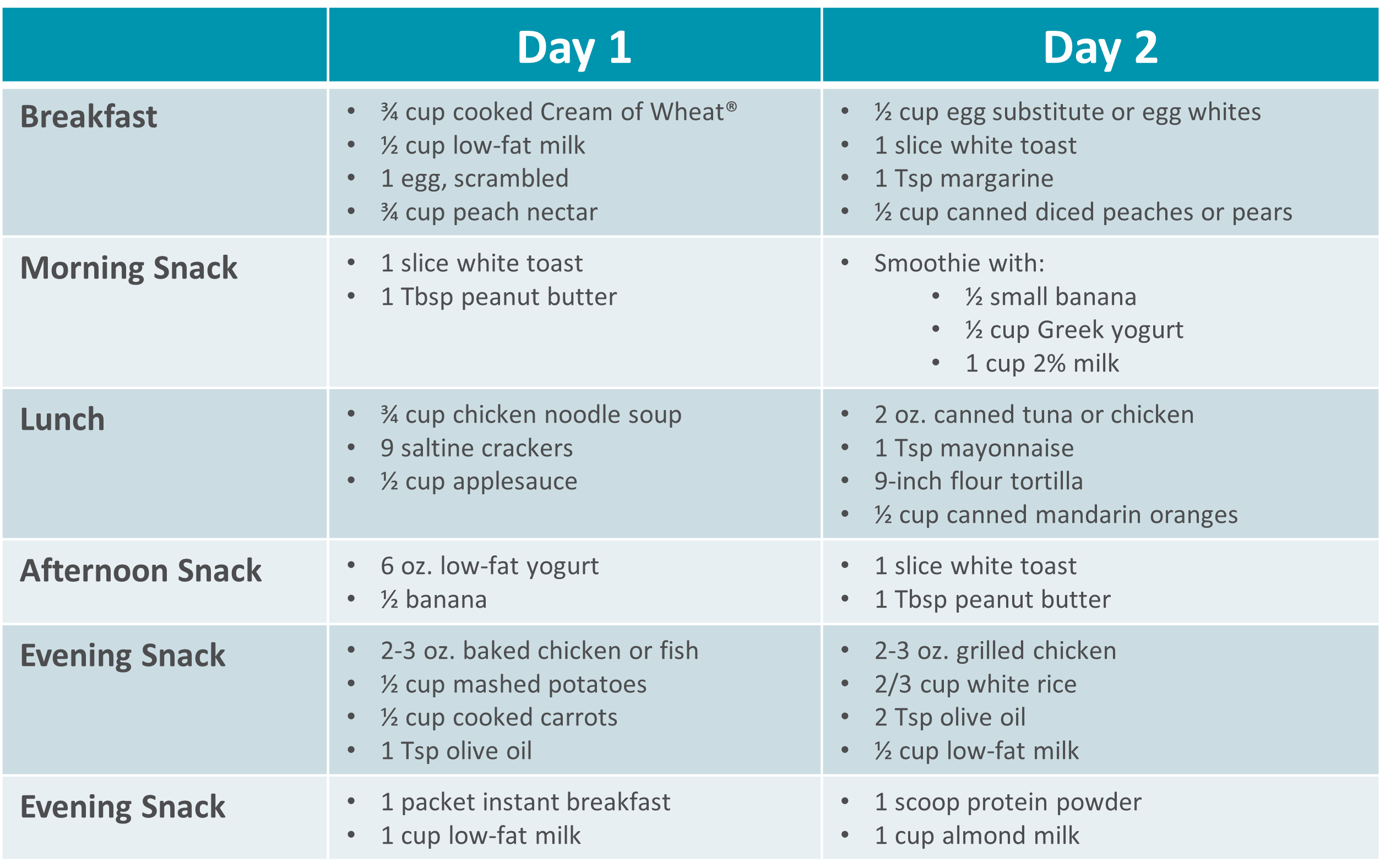 |
Please visit Restore+ to learn more about the nutrition support services offered by Option Care Health.
*This material is for informational purposes only. It does not replace the advice or counsel of a healthcare professional. Please consult with your Registered Dietitian for more detailed, individualized information.

营养支持
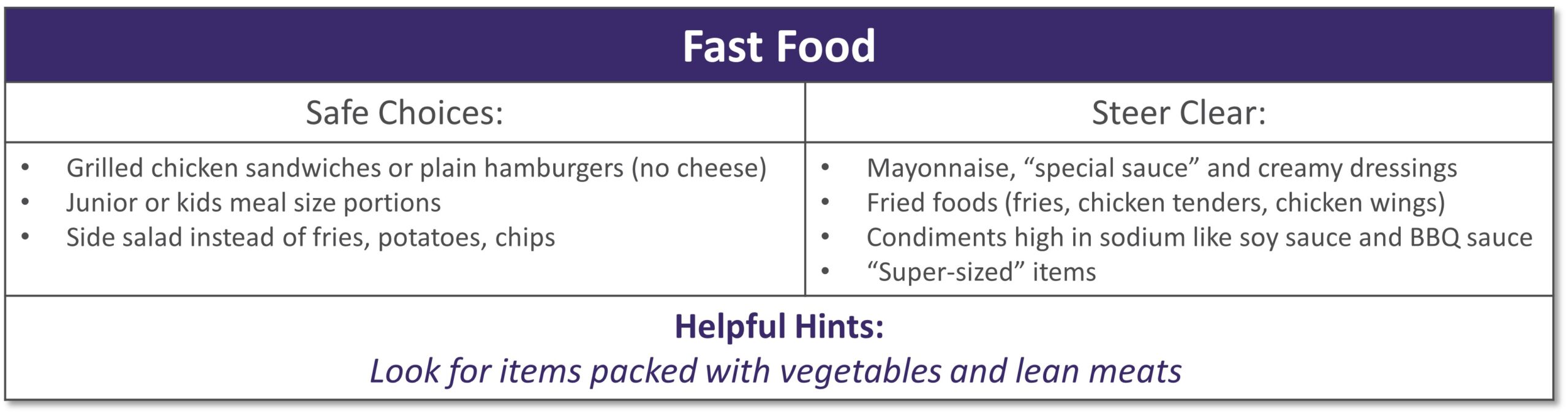
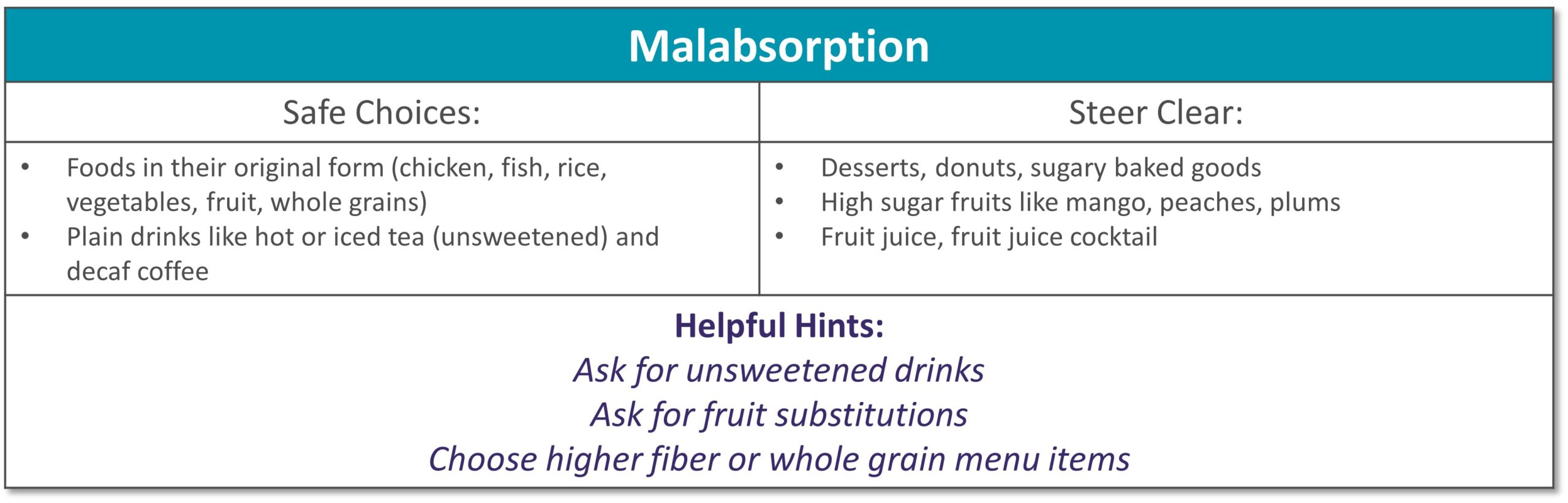
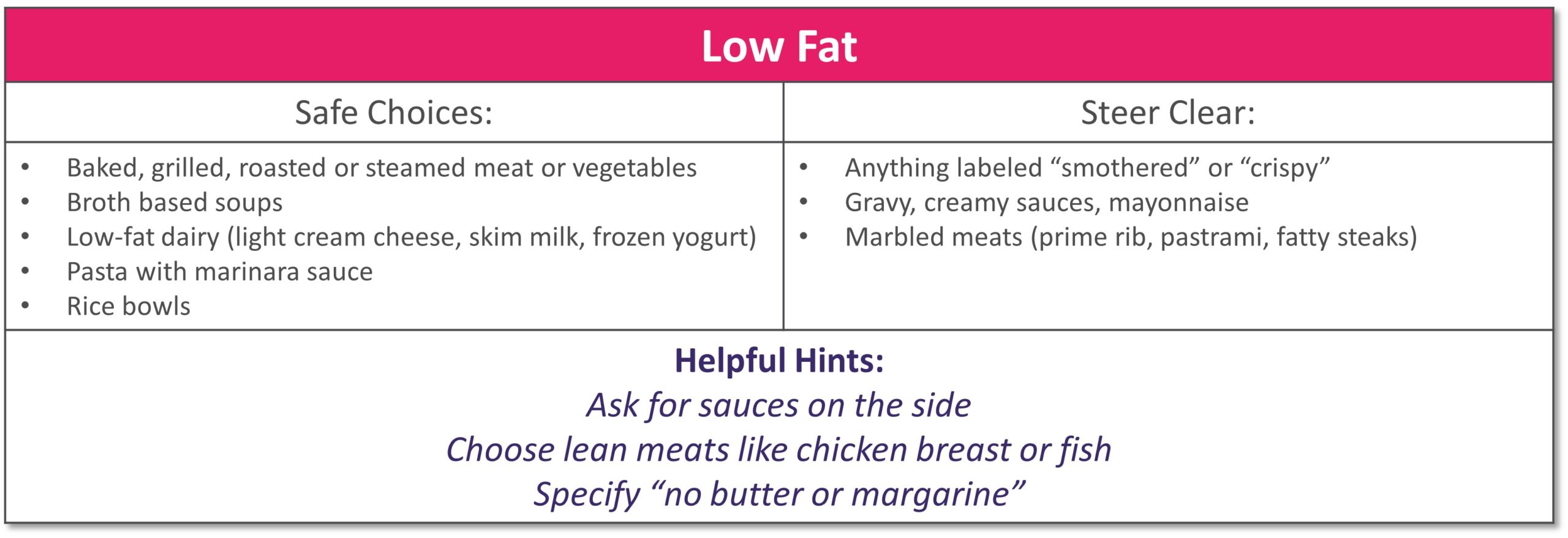
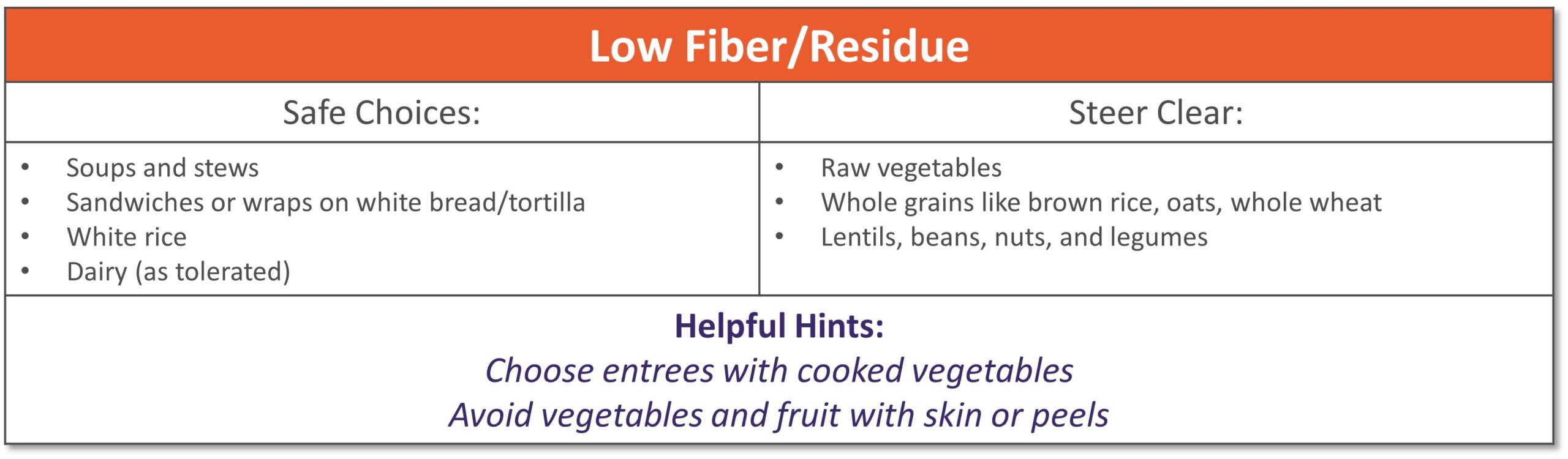
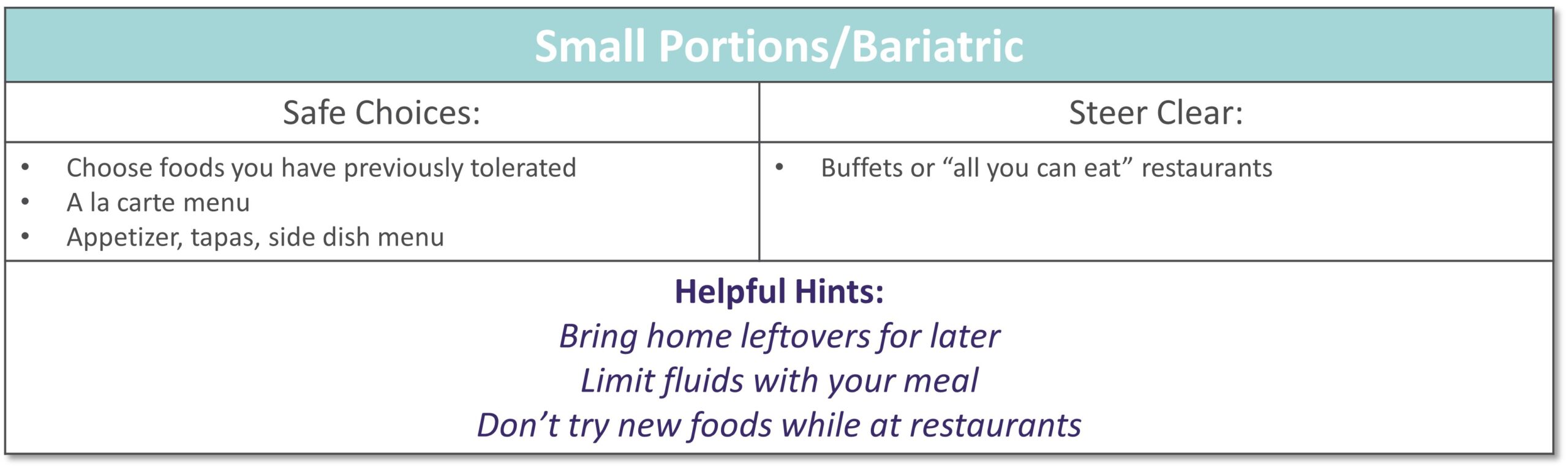
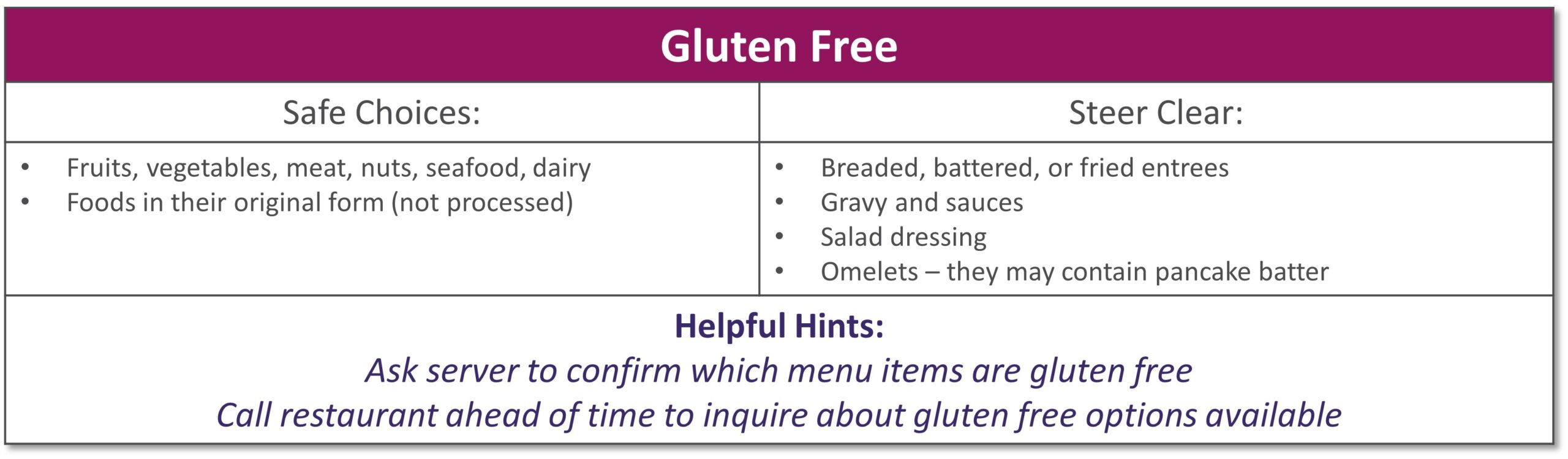
Dining out at restaurants is a nice treat but also challenging when trying to stick with your therapeutic diet, especially with gastrointestinal diseases. Most restaurants have menus and nutritional information available online. Restaurants are not required to have nutrition information available if they have less than 20 locations. Follow these tips to navigate eating out if you have specialized nutrition needs.
GENERAL TIPS:
- Research the menu online
- Pick a cuisine you tolerate
- Ask server for nutritional information or ingredients if not listed on the menu
- Do NOT be afraid to ask to customize the meal or ask for specific changes
- Communicate with wait staff if you have a food allergy or intolerance
- HAVE A PLAN AND STICK WITH IT!
|
|
|
|
|
|
|
|
|
|
|
|
|
Please visit Restore+ to learn more about the nutrition support services offered by Option Care Health. *This material is for informational purposes only. It does not replace the advice or counsel of a healthcare professional. Please consult with your Registered Dietitian for more detailed, individualized information. |

营养支持
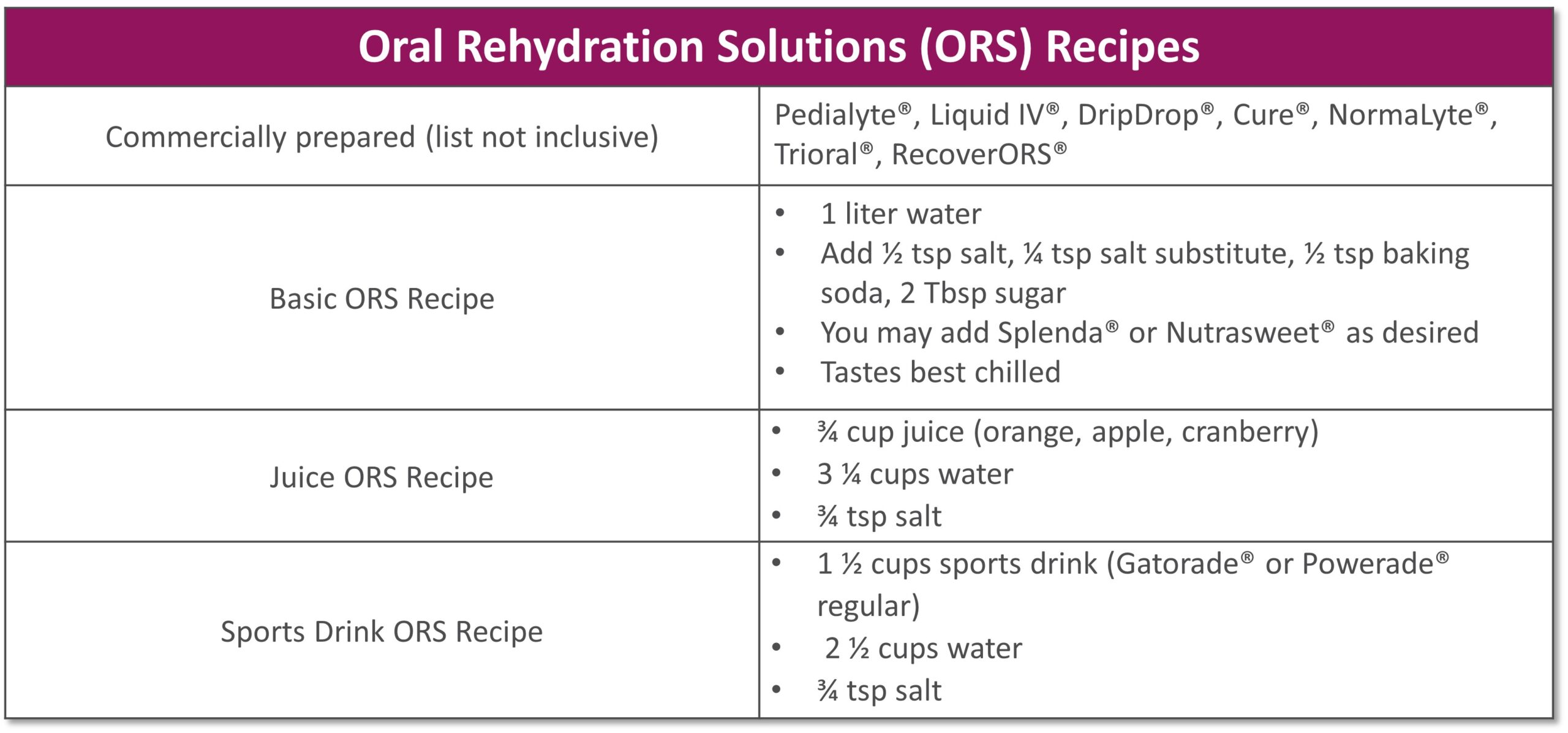
Short bowel syndrome (SBS), or intestinal failure, is a condition in which your body is unable to absorb enough nutrients from foods and fluids you consume. This can occur after a surgical resection or damage to your intestines. Symptoms and absorption vary by individual based on the amount and health of the remaining intestine. Symptoms of SBS can include diarrhea, dehydration, electrolyte abnormalities, and weight loss.
The following tips are intended to maximize absorption, improve your nutritional status and reduce dependence on parenteral nutrition.
- Mealtime
- Eat small, frequent meals (6-8 per day)
- Foods
- Eat protein at all meals: eggs, creamy peanut butter, chicken, fish, beef, tofu
- Choose complex carbohydrates such as bread, pasta, rice, and potatoes
- Limit raw vegetables to small amounts
- Avoid fruits with skin or edible seeds
- Limit raw fruits to very small portion twice a day
- Increase your soluble fiber to thicken output with foods such as bananas, applesauce, rice, oatmeal or use of soluble fiber supplements
- Avoid high fat foods such as fried foods if your colon is intact
- Use caution with dairy products – lactose intolerance is common with SBS
- Avoid concentrated sweets such as candy, desserts, and juice
- Avoid foods artificially sweetened with sorbitol or mannitol (Splenda® is okay)
- Fluids
- Drink isotonic fluids (with electrolytes), ideally oral rehydration solutions (see recipes below)
- Do not drink fluids with meals as it increases how quickly food passes through
- Limit to 4 oz. fluid during your meal to allow your food to be best absorbed
- Drink ½ hour before or 2 hours after eating
- If you do not have your colon, your fluid losses will be higher
- 其他
- If prescribed by your doctor, take antidiarrheal medication ½ hour before meals
- Salty foods such as pretzels or soups are usually well tolerated and help absorb fluid
- Avoid caffeine and alcohol
See below for help in choosing more optimal foods from each food group:
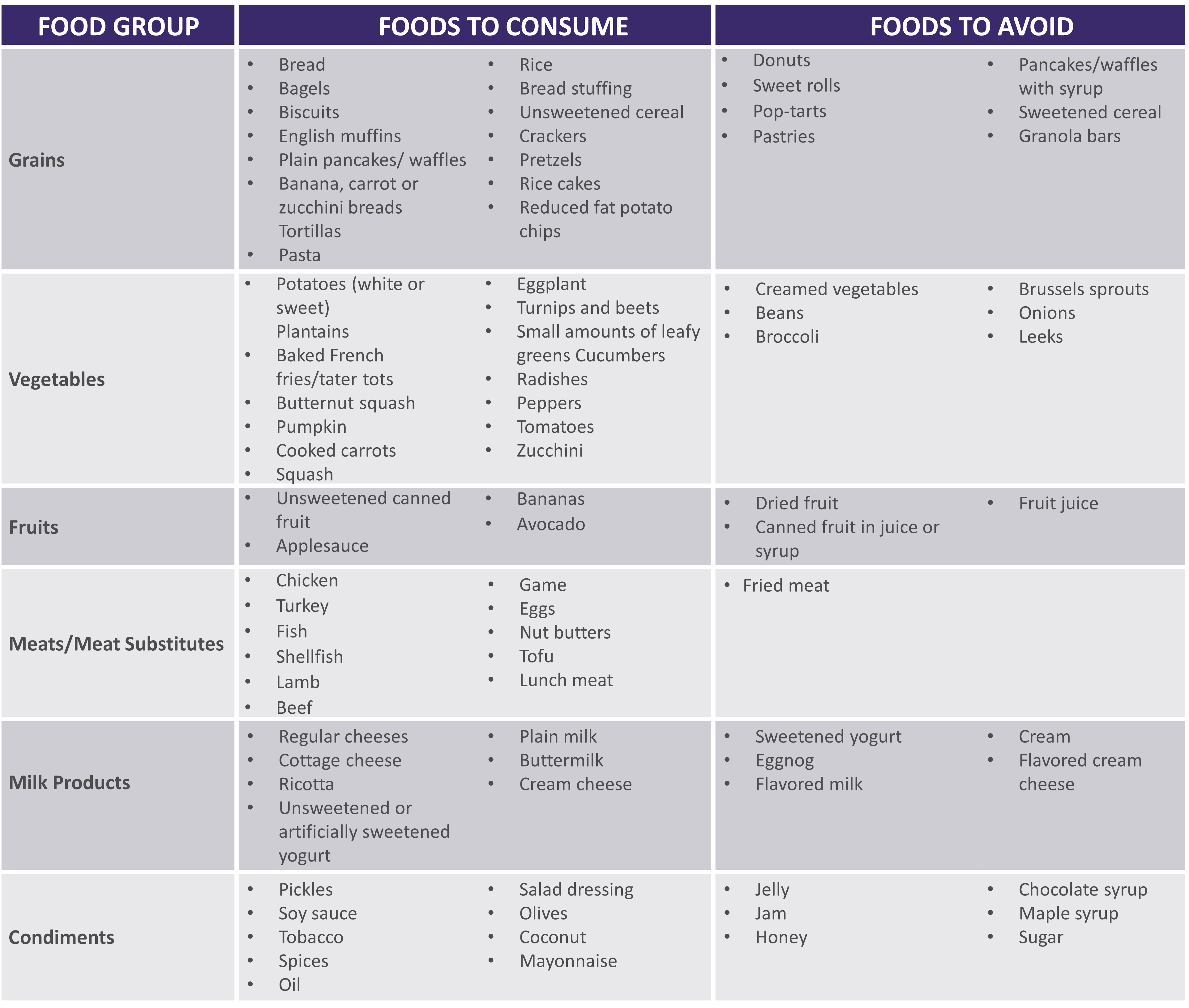 |
|
|
|
**For homemade ORS, discard after 24 hours if not consumed **Visit for more recipes: https://optioncarehealth.com/patients/resources/sbs-friendly-recipes |
SBS Sample Menu |
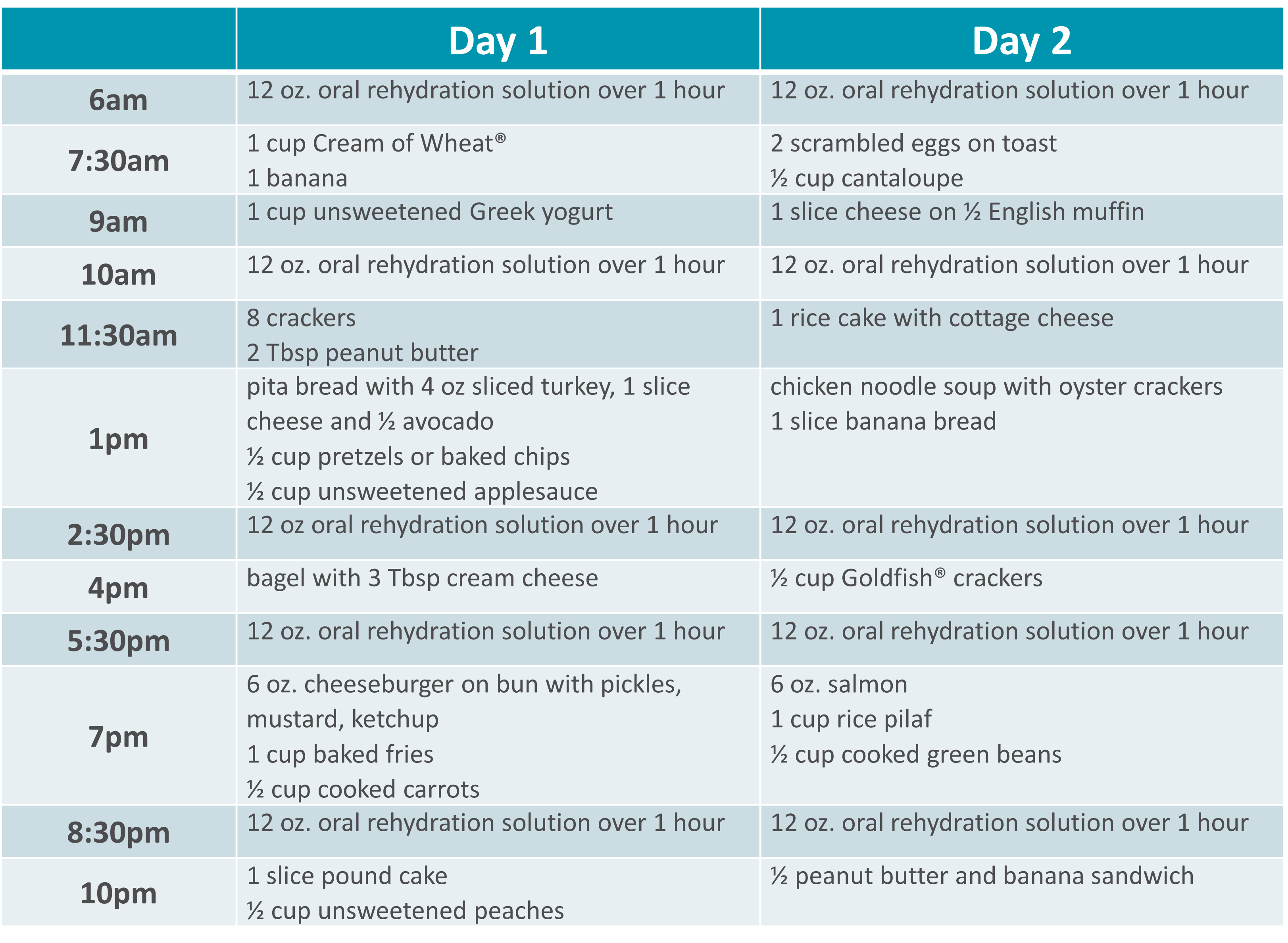 |
Please visit Restore+ to learn more about the nutrition support services offered by Option Care Health.
*This material is for informational purposes only. It does not replace the advice or counsel of a healthcare professional. Please consult with your Registered Dietitian for more detailed, individualized information.

营养支持
Gillian was just 11 years old when she began treatment for multiple complex chronic illnesses. As a teenager, she was diagnosed with gastrointestinal (GI) motility disorder and gastroparesis, which led to long-term, severe malnutrition.
“It was really hard missing out on so many activities growing up. I was prescribed various medications and tube feedings, but nothing helped long term. By early adulthood my symptoms worsened so I had to withdraw from college and take an extended medical leave from my job,” she said.
From 2015 to 2018, Gillian’s health progressively declined. “I was on tube feeds and other intravenous (IV) medications at the time. I began losing weight again, my neurological function was declining and I couldn’t speak or walk.” As Gillian’s health continued to decline, she found the strength to advocate for herself and build upon her excellent team of healthcare providers.
Gillian was put on total parenteral nutrition (TPN) in 2018, managed by Option Care Health. “This was my turning point. Today my labs are perfect and my cognitive function is back to normal. My weight has stabilized and I’m back to living life. I owe so much of my progress to my Option Care Health team.” Gillian continued, “My registered dietitian (RD) is amazing. During the initial COVID outbreak, I was struggling with my health and I couldn’t reach my doctors, but my Option Care Health RD was there every time I reached out. I got the help I needed and I owe it all to her.”
She claims that her Option Care Health team including her pharmacist and pharmacy technician go above and beyond expectation. “Other companies and even providers don’t always focus on how the patient needs to be living their best quality of life during treatment. My team at Option Care Health set up my deliveries in the evening to accommodate my work schedule. They also deliver them upstairs to me because I’m unable to carry them. My pharmacist and tech were so helpful this summer. They were able to find a way for me to go on vacation by switching around my infusions and supplies. Thanks to their help, I was able to go on my first trip since 2015! They are really focused on me as a person, not just a patient.”
Her message to her Option Care Health team is one of gratitude, “I just want them all to know how appreciative I am. They have and continue to be a key part of my recovery and I couldn’t be more grateful.” Gillian is thriving and living her best quality of life. She’s working, volunteering and spending as much time as possible with family and friends.
Learn more about malnutrition and join us in spreading awareness this ASPEN Malnutrition Awareness Week*, September 19th-23rd: ASPENMAW22
*Malnutrition Awareness Week™ 是美国肠外和肠内营养协会(ASPEN)的一个注册标志。经 ASPEN 许可使用。

营养支持
 临床营养不是单方面的努力。
临床营养不是单方面的努力。
在 Option Care Health,我们的注册营养师是营养支持团队的重要组成部分,与护士、药剂师和其他临床医师共同努力,无论在医院还是在家中,都能为我们的患者提供最佳护理。
我们专注于协作方法,因为我们知道它对患者最有效并支持最佳疗效。
点击以下链接阅读 Today’s Dietitian 刊登的文章。

营养支持
After overcoming ovarian cancer in 1995, retired nurse Lydia Zwilling found herself facing an arduous battle to reclaim her health. Nearly a quarter million women are diagnosed with ovarian cancer every year and for most, treatment goes according to plan. Unfortunately, some like Lydia, experience complications that last a lifetime.
While radiation therapy may have saved Lydia’s life, it also burned her small intestine and contributed to complications that ultimately caused her kidneys to fail. She had to be put on dialysis for two years before she was able to receive a kidney transplant in 2006.
Doctors also had to remove the burned portion of her small intestine, leaving her with just three functioning feet of her bowel. Diagnosed with short bowel syndrome (SBS), Lydia started to experience dramatic weight loss because her body could no longer absorb adequate nutrition. At 72 pounds, she was emaciated and unable to regain any weight. She became home-bound.
“I felt deeply frustrated,” Lydia said. “After beating a life-threatening cancer, I still had no strength or energy. I decided it was time to take some action to see what could make me better.”
In 2006, Lydia was introduced to Option Care by her attending physician and put on total parenteral nutrition (TPN), which gives her the nutrition she needs through intravenous delivery.
“TPN made an immediate difference in my overall health,” Lydia said. “I finally started to feel like myself again.”
Lydia and her husband are registered nurses so they are able to handle her TPN treatments and labs from home, self-infusing five days a week for nine hours at night. Lydia works closely with her care team at Option Care to receive additional antibiotics when she needs them. They also coordinate directly with her physicians to communicate any changes in her treatment.
“After many years with Option Care as my infusion provider, I’ve developed a close relationship with my care team and we’ve gotten to know each other on a personal level,” Lydia said. “You can tell that they care about what is going on with me and not just my medical health. I have complete confidence in their abilities to provide me with the best care possible.”
As a grateful cancer survivor, Lydia is thriving thanks to TPN. She credits her involvement with Option Care as enabling her to regain a near normal life. She is now able to visit her grandchildren who live six and a half hours away as well as escape the cold Minnesota winters for vacations in Florida and Arizona. Option Care supports Lydia by working with her to ensure she has access to necessary medications while she’s traveling.
“I can get out and get back a little bit of my life that I had before,” Lydia said. “It’s important to spend your energy on trying to get yourself better. Option Care home infusion helps me do that.”

营养支持
PHOENIX, March 21, 2019 — Clinical interventions provided by a nutrition support team can prevent hospital readmission in patients with short bowel syndrome (SBS) receiving home parenteral nutrition (PN), saving millions in costs annually, suggests a study[*]Englert M, Stodola K. Proactive Interventions by Nutrition Support Clinicians in Patients with Short Bowel Syndrome (SBS) on Home Parenteral Nutrition (HPN) Results in Decreased Hospitalizations and Improved Financial Outcomes. Abstract presented at the American Society for Parenteral and Enteral Nutrition (ASPEN) 2019 Nutrition Science & Practice Conference; March 23-26, 2019, Phoenix. by Option Care Enterprises, Inc. ( “Option Care”), the nation’s leading provider of home and alternate site infusion therapy services. The research is being presented at the American Society for Parenteral and Enteral Nutrition (ASPEN) 2019 Nutrition Science & Practice Conference and was chosen as an Abstract of Distinction.
Among SBS patients receiving home PN provided intravenously (IV), dehydration is a common cause of hospital readmission, with an average three-day length of stay. In the study, the nutrition support team — including a dietitian, nurse and pharmacist — made recommendations (interventions) to adjust the home PN volume based on the weekly monitoring of patients’ hydration status through reviewing laboratory values and conducting nutrition assessments.
“Home nutrition patients on PN with SBS need to be observed closely the first month to prevent dehydration and making appropriate adjustments to the home PN volume is essential,” said Mary Englert, MS, RD, CSO, LDN, CNSC, Area Lead, Nutrition Support Dietitian at Option Care and lead author of the study. “Every intervention decreases the likelihood of the patient being readmitted to the hospital and this study highlights the value of a nutrition team in providing clinical monitoring and nutrition support, which leads to improved patient care and significant cost savings.”
The study included 116 patients with SBS who received home PN after being discharged from the hospital. The Registered Dietitian-led nutrition support team provided ongoing evaluation by reviewing labs weekly and conducting a thorough nutrition assessment, recommending adjustments to the volume of PN when indicated for a total of 63 proactive interventions during the four-week review period. The most common reasons for home PN volume adjustments were: to meet the patient’s estimated fluid needs (56 percent); lab values reflecting dehydration (22 percent) and increased gastrointestinal output (22 percent).
Only 14 of the study patients were readmitted to the hospital within two weeks of discharge, none resulting from dehydration. Readmissions were due to: abscess/infection not related to PN (35.7 percent); line infection/replacement (21.4 percent); bowel obstruction (14.3 percent) and nausea/vomiting, feeding tube replacement, chest pain and unknown (7.1 percent each).
The researchers determined the interventions correlated to 189 hospital days prevented and $378,000 in costs saved in one month. Projected over one year that equates to 2,268 hospital days prevented and over $4.5 million in savings.
Also presented at ASPEN:
In another Option Care study[*]Hughey M, Corey B. Early Clinical Intervention Increases Compliance and Decreases Unnecessary Discontinuation in SBS Patients treated with Teduglutide. Abstract presented at the American Society for Parenteral and Enteral Nutrition (ASPEN) 2019 Nutrition Science & Practice Conference; March 23-26, 2019, Phoenix. presented at ASPEN, 162 SBS patients were proactively screened for appropriate dosing before receiving teduglutide, which helps increase fluid and nutrient absorption resulting in decreased dependence on Parenteral Support. The clinical intervention resulted in recommended reductions to the prescribed dose in 64 of the patients (40 percent), half of which were based on impaired kidney function. Ensuring patients receive the appropriate dose reduces potential therapy complications including fluid overload, worsening kidney function and premature therapy discontinuation.
关于 Option Care
Option Care Enterprises, Inc. (Option Care) is the nation’s leading and most trusted provider of home and alternate site infusion therapy services. Holding accreditations from industry quality organizations ACHC, PCAB, ASHP and URAC,[*]Accreditation Commission for Health Care (ACHC), Pharmacy Compounding Accreditation Board (PCAB), American Society of Health-System Pharmacists (ASHP) and URAC the company draws on nearly 40 years of clinical care experience to offer patient-centered therapy management. Option Care’s signature infusion services include the clinical management of infusion medicines, nursing support and care coordination. Option Care’s multidisciplinary team of more than 1,800 clinicians — including pharmacists, nurses and dietitians — are able to provide infusion service coverage for nearly all patients across the United States needing treatment for complex and chronic conditions. Learn more at www.OptionCare.com.

营养支持
Option Care 研究发现,患者经常被开出不符合其需求的家庭营养处方
临床营养周上提出的研究表明,未经调整的医嘱会导致喂食过量、喂食不足、健康风险、增加成本
 ORLANDO, Fla., Feb. 9, 2017 — Nutrition support orders upon discharge from the hospital often don’t meet the needs of patients, according to Option Care data being presented at the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Clinical Nutrition Week (CNW) conference. If nutrition support orders are not corrected, patients may be overfed or underfed, both of which put them at health risk and in the case of overfeeding, adds unnecessary costs.
ORLANDO, Fla., Feb. 9, 2017 — Nutrition support orders upon discharge from the hospital often don’t meet the needs of patients, according to Option Care data being presented at the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Clinical Nutrition Week (CNW) conference. If nutrition support orders are not corrected, patients may be overfed or underfed, both of which put them at health risk and in the case of overfeeding, adds unnecessary costs.
Option Care 研究人员确定,在将近四分之一的情况下,家庭肠外(静脉注射)营养 (HPN) 患者出院时的医嘱未能满足患者的需求。虽然家庭肠内(喂食管)营养 (HEN) 患者的营养需求更有可能得到满足,但是 38% 的医嘱无法满足流体(水分)需求。Option Care 注册营养师在患者出院回家接受护理时检查了所有医嘱,进行了营养评估,并且基于患者的实验室数据、活动水平和整体病况,在必要时建议对营养医嘱加以修改。
“Nutrition support is complex and quality patient care provided in the home setting requires close collaboration between referring clinicians and a qualified home nutrition support team that has nutrition support expertise, including a registered dietitian, pharmacist and nurse,” said Noreen Luszcz, RD, MBA, CNSC, lead author of the study and nutrition program director for Option Care. “When a patient leaves the hospital, it is vital that the home infusion dietitian complete a nutrition assessment to ensure the order follows A.S.P.E.N. guidelines and the patient’s current needs are being met.”
喂食过量所提供的营养超出要求,从而引起代谢问题,导致体重过度增加,并且增加成本。喂食不足的患者则可能无法充分地增加体重或尽快痊愈。
因卓越和创新而荣获 A.S.P.E.N. CNW “杰出海报奖”的这项研究包含了对 187 名 HPN 患者和 349 名 HEN 患者的营养处方分析
这些患者在出院时没有专门的营养支持团队来指导开处方。
对于 187 名 Option Care HPN 患者,研究人员确定,原医嘱在平均 23% 的情况下不符合患者的需求。他们发现:
- 41 例 (22%) 未达到流体需求;
- 48 例 (26%) 未达到氨基酸(蛋白质)需求;
- 39 例 (21%) 未达到葡萄糖(碳水化合物)需求;
- 34 例 (18%) 未达到脂质(脂肪)需求;
- 51 例 (27%) 未达到总热量需求。
此外,24 名患者 (13%) 被不当地规定接受 HPN,他们本应该通过其他成本更低的途径来获得营养,如 HEN 和/或口服摄入。HPN 只应适用于胃肠道系统无法充分处理营养物质的患者。开具处方最多的医师排名前两位是内科医师 (29%) 和胃肠病医师 (19%)。
在蛋白质方面,最初的医嘱可能会导致在 48% 的情况下出现喂食过量,在 52% 的情况下出现喂食不足。在剩余的类别中,最初的医嘱更有可能使患者出现喂食不足的情况。研究人员估计,过量规定服用蛋白质的平均含量将会给每名接受 90 天(治疗的平均时长)HPN 治疗的患者额外增加 179,837 美元。他们确定,光是纠正 12% 的 HPN 医嘱的蛋白质处方这一项,就能节省 520 万美元的医疗保险成本。
在 349 名 Option Care HEN 患者中,研究人员评估了原医嘱,确定:
- 133 例 (38%) 不含水冲洗医嘱(因此患者无法获得足够的流体);
- 15 例 (4%) 的处方并不是最适合其病况的配方;
- 10 例 (2%) 会出现喂食过量的情况;
- 18 例 (5%) 会出现喂食不足的情况。
研究人员指出,各种各样的因素可能会导致出院时的营养医嘱无法满足患者的需求。医师经常给患者开药,但这些医师可能缺乏营养专科的专业知识,也没有一支合格的营养支持团队(包括注册营养师、护士和药剂师)来引导他们。此外,营养需求会随着时间的推移而发生变化。急性损伤患者可能在愈合期需要补充更多的蛋白质,但到了患者出院回家时,这种需求会随之减少。如果未对医嘱进行调整,患者就会摄入不适当的蛋白质含量,随着时间的推移就会积少成多。最后,到了确定患者是否有资格接受家庭营养支持时,就会进行大量的审查(Medicare 尤其如此),与医院的审查标准不同。
Option Care 的营养支持项目遵循一个多学科团队的护理方法,该团队包括输液护士、药剂师和获得营养支持认证的营养师,他们与医师密切合作,为 HPN 和 HEN 患者提供最高品质的护理。全美各地的每个护理管理中心都有一名注册营养师提供支持。
患者被开出 HPN 或 HEN 的处方,是因为他们具有如癌症、中风、胃肠道疾病或手术并发症等病症,无法通过口服来满足他们的营养需求。虽然这两种疗法可以在医院进行临时施用,但每年大约有 40,000 名 HPN 患者和 344,000 名 HEN 患者在家中安全地接受营养治疗,费用更低,避免了医院获得性感染的风险,可重返工作并且过着积极向上的生活。尽管有些人是短期接受这些治疗,但许多人的治疗时间更长,有些甚至是终生治疗。
关于 Option Care
Option Care Enterprises, Inc. (Option Care) 是全美最大和最值得信赖的家庭和备选医疗站点输液服务提供者。作为行业领导者,本公司汲取了近 40 年的临床护理经验,提供以患者为中心的治疗管理。Option Care 的标志性家庭输液+服务包括输液药物的临床管理、护理支持和护理协调。Option Care 由 1,700 多名临床从业人员(包括药剂师、护士和营养师)组成的多学科团队能够为美国各地需要接受复杂和慢性病治疗的几乎所有患者提供家庭输液服务覆盖。有关详情请访问 www.OptionCare.com。

营养支持
Many Home Parenteral Nutrition Patients Denied Medicare Reimbursement 尽管接受了 A.S.P.E.N.指导方针导向治疗
Option Care 研究强调需要将护理和承保范围相结合
 ORLANDO, Fla., Feb. 9, 2017 — Many home parenteral nutrition (HPN) patients who struggle to gain or maintain weight due to complex medical conditions may be falling through the cracks due to an outdated Medicare qualification process, suggests Option Care research being presented at the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Clinical Nutrition Week (CNW) conference. The study determined that Medicare coverage often doesn’t match up with A.S.P.E.N. guideline recommendations, forcing patients to pay for some or all of their life-saving care.
ORLANDO, Fla., Feb. 9, 2017 — Many home parenteral nutrition (HPN) patients who struggle to gain or maintain weight due to complex medical conditions may be falling through the cracks due to an outdated Medicare qualification process, suggests Option Care research being presented at the American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.) Clinical Nutrition Week (CNW) conference. The study determined that Medicare coverage often doesn’t match up with A.S.P.E.N. guideline recommendations, forcing patients to pay for some or all of their life-saving care.
研究人员发现,超过一半的 HPN(静脉输液)患者的护理符合 A.S.P.E.N. 指导方针,但却不符合 Medicare 的承保资格。这些研究结果表明,Medicare 采用了过时的 HPN 资格标准,包括无法体现当前推荐治疗的营养不良诊断工具。
“HPN is an expensive therapy and understandably Medicare wants to ensure that patients require that level of nutrition,” said Natalie S. Tu, RD, lead author of the study and clinical nutrition support dietitian for Option Care. “However, many malnourished patients have a clear need for HPN but don’t qualify for Medicare coverage. Care team members — including doctors and dietitians — need to diligently document the patient’s need in an attempt to secure Medicare coverage.”
In some cases, appeals providing additional documentation of need may be successful in securing coverage for patients initially denied by Medicare. Medicare patients who don’t qualify for coverage pay out of pocket costs which can be up to $250 a day and are prohibitive for many people. The average length of therapy for Option Care HPN patients is three months.[*] Option Care data on file.Patients who have supplemental insurance may be partially covered, but will be required to pay a daily deductible, which also adds up.
目前,大约 20% 的 Option Care 家庭肠外营养 (HPN) 患者有联邦医疗保险 (Medicare)。随着人口的老龄化,这一比例将会继续增加,突显了 Medicare 保险与 A.S.P.E.N. 指导方针应更好地保持一致的需求,Tu 说道。
这项 Option Care 研究因其卓越与创新被提名为 A.S.P.E.N. 临床营养周 (CNW) 优秀论文摘要。研究人员分析了接受 HPN 治疗的 142 名患者,确定有 49 人 (35%) 符合 Medicare 的 HPN 资格标准,56 人 (39%) 不符合标准,而 37 人 (26%) 则停滞不前,因为资格审查过程中断或未完成。在 56 名没有资格获得联邦医疗保险 (Medicare) 的患者中,31 人 (55%) 确实达到了 A.S.P.E.N. 指导方针推荐。
患者被开出 HPN 的处方,是因为他们具有如癌症、中风、胃肠道疾病或手术并发症等病症,无法通过口服或喂食管(肠内营养)来满足他们的营养需求。虽然 HPN 可以在医院进行施用,但每年大约有 40,000 名患者在家中安全地接受营养治疗,费用更低,避免了医院获得性感染的风险,可重返工作并且过着积极向上的生活。
Option Care 的营养支持项目遵循一个多学科团队的护理方法,该团队包括输液护士、药剂师和获得营养支持认证的营养师,他们与医师密切合作,为家庭营养患者提供最高品质的护理。全美各地的每个护理管理中心都有一名注册营养师提供支持。
关于 Option Care
Option Care Enterprises, Inc. (Option Care) is one of the nation’s largest and most trusted providers of home and alternate treatment site infusion services. An industry leader, the company draws on nearly 40 years of clinical care experience to offer patient-centered therapy management. Option Care’s signature Home Infusion Plus services include the clinical management of infusion medicines, nursing support and care coordination. Option Care’s multidisciplinary team of more than 1,800 clinicians — including pharmacists, nurses and dietitians — are able to provide home infusion service coverage for nearly all patients across the United States needing treatment for complex and chronic conditions. Learn more at www.OptionCare.com.
# # #